Скачать с ютуб 8 Simple Steps Towards Mental Health Billing в хорошем качестве
Скачать бесплатно и смотреть ютуб-видео без блокировок 8 Simple Steps Towards Mental Health Billing в качестве 4к (2к / 1080p)
У нас вы можете посмотреть бесплатно 8 Simple Steps Towards Mental Health Billing или скачать в максимальном доступном качестве, которое было загружено на ютуб. Для скачивания выберите вариант из формы ниже:
Загрузить музыку / рингтон 8 Simple Steps Towards Mental Health Billing в формате MP3:
Если кнопки скачивания не
загрузились
НАЖМИТЕ ЗДЕСЬ или обновите страницу
Если возникают проблемы со скачиванием, пожалуйста напишите в поддержку по адресу внизу
страницы.
Спасибо за использование сервиса savevideohd.ru
8 Simple Steps Towards Mental Health Billing
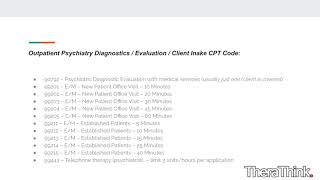
Mental health billing isn’t easy. If it was…you probably wouldn’t be watching this video. As a behavioral health entity, your main goal isn’t to collect money from your patients…it’s to help treat them. Unfortunately, though, many behavioral health organizations have no choice but to spend countless hours on the billing side…because there’s so much involved. At the end of the day, billing is what keeps your doors open as a behavioral health organization. LINKS: ____________________________________________ https://etactics.com/blog/mental-heal... ____________________________________________ It’s possible why so many mental health practices and facilities find billing so difficult isn’t because it’s impossible, but because they haven’t streamlined their process. The first step in the mental health billing process is information collection. You can’t bill for your services without collecting information from your clients. That might sound like an obvious statement, but it’s trickier than it sounds. What information do you need to collect from your mental health clients for billing purposes? You need to be able to provide the following information on your end…Provider Tax ID, Employment Identification Number or Social Security Number, Individual Provider NPI, Organizational Group NPI, Provider License, and Address. There are only 4 pieces of patient demographic information you need at a minimum for billing purposes…Full legal name, Date of birth, Address, and Gender. Beyond demographic information, you gather the following patient insurance information…Card Member or Subscriber ID, Group number, Authorization Number, Claims address, and Mental Health/Behavioral health provider phone number (the eligibility one). The second step is information verification and eligibility. Gathering the information from your clients is only the first step, it’s also your responsibility to ensure that it’s accurate, up-to-date and eligible. In a streamlined mental health organization, this process kicks off the moment the patient walks through the doors for their visit and continues through their appointment. This is a key step in the process, verifying eligibility early helps stop this type of denials months before you would receive them. You can call the patient’s provider to verify eligibility but that takes time. Instead, there are many systems that can check eligibility on your behalf in a more efficient manner than making phone calls. This technology could be supplied by your EHR, clearinghouse, or a different third-party. Third is CPT code recording. CPT codes are essential to billing. Without them, the payer wouldn’t be able to understand what happened during your client’s visit. Recording them must happen right after the appointment occurs. The four most common CPT codes are…90791 which Exclusive to the first appointment held with a client… 90832 for a 16 - 37 minute session… 90834 for a 38-52 minute session…and 90837 for a 53+ minute session. Although it seems straightforward, it’s worth mentioning that you bill for the first appointment first and then refer to the other codes based on session length. Fourth is claim submission. There are many different techniques you could use to submit your claims but the best option a total package claim submission portal and clearinghouse provider. These clearinghouses (like ours) can automatically accomplish multiple claim submission process alternatives for every unique scenario. That way, if a client comes through with a payer that only accepts paper claim submissions, you let the clearinghouse know and it will automatically generate and mail a CMS 1500 or UB-04 form. Oh, and it also integrates with your PM/EHR system and vice versa. — Step five…clearinghouse rejections. Before you “officially” send your claims to your client’s payers your clearinghouse should help you out via scrubbing and rejections. Both of those are processes that I alluded to in those term’s definitions but this is a good place to mention them again. Your clearinghouse's sole purpose is to “have your back” when it comes to mental health billing. That means it should be able to alert you of errors you make during the claim submission process and correct the same automatically. This step happens simultaneously with step 4, but it needs mentioning because it’s another added benefit of choosing the total package claim submission portal and clearinghouse provider. ► Reach out to Etactics @ https://www.etactics.com ►Subscribe: https://rb.gy/pso1fq to learn more tips and tricks in healthcare, health IT, and cybersecurity. ►Find us on LinkedIn: / etactics-inc ►Find us on Facebook: / #MentalHealthBilling