Urticaria: Classification, Pathogenesis, Clinical Features, Treatment —Б–Ї–∞—З–∞—В—М –≤ —Е–Њ—А–Њ—И–µ–Љ –Ї–∞—З–µ—Б—В–≤–µ
urticaria
urticaria causes
urticaria treatment
what is urticaria
causes of urticaria
urticaria symptoms
urticaria symptoms and treatment
urticaria usmle lecture dermatology
urticaria lecture usmle
treatment urticaria
urticaria dermatology
urticaria usmle
urticaria neetpg
acute urticaria
chronic urticaria
treatment for urticaria
urticaria usmle dermatology lecture
urticaria neetpg lecture for neetpg
urticarial rash
chronic spontaneous urticaria
usmle step 1
–Я–Њ–≤—В–Њ—А—П–µ–Љ –њ–Њ–њ—Л—В–Ї—Г...
–°–Ї–∞—З–∞—В—М –≤–Є–і–µ–Њ —Б —О—В—Г–± –њ–Њ —Б—Б—Л–ї–Ї–µ –Є–ї–Є —Б–Љ–Њ—В—А–µ—В—М –±–µ–Ј –±–ї–Њ–Ї–Є—А–Њ–≤–Њ–Ї –љ–∞ —Б–∞–є—В–µ: Urticaria: Classification, Pathogenesis, Clinical Features, Treatment –≤ –Ї–∞—З–µ—Б—В–≤–µ 4k
–£ –љ–∞—Б –≤—Л –Љ–Њ–ґ–µ—В–µ –њ–Њ—Б–Љ–Њ—В—А–µ—В—М –±–µ—Б–њ–ї–∞—В–љ–Њ Urticaria: Classification, Pathogenesis, Clinical Features, Treatment –Є–ї–Є —Б–Ї–∞—З–∞—В—М –≤ –Љ–∞–Ї—Б–Є–Љ–∞–ї—М–љ–Њ–Љ –і–Њ—Б—В—Г–њ–љ–Њ–Љ –Ї–∞—З–µ—Б—В–≤–µ, –≤–Є–і–µ–Њ –Ї–Њ—В–Њ—А–Њ–µ –±—Л–ї–Њ –Ј–∞–≥—А—Г–ґ–µ–љ–Њ –љ–∞ —О—В—Г–±. –Ф–ї—П –Ј–∞–≥—А—Г–Ј–Ї–Є –≤—Л–±–µ—А–Є—В–µ –≤–∞—А–Є–∞–љ—В –Є–Ј —Д–Њ—А–Љ—Л –љ–Є–ґ–µ:
-
–Ш–љ—Д–Њ—А–Љ–∞—Ж–Є—П –њ–Њ –Ј–∞–≥—А—Г–Ј–Ї–µ:
–°–Ї–∞—З–∞—В—М mp3 —Б —О—В—Г–±–∞ –Њ—В–і–µ–ї—М–љ—Л–Љ —Д–∞–є–ї–Њ–Љ. –С–µ—Б–њ–ї–∞—В–љ—Л–є —А–Є–љ–≥—В–Њ–љ Urticaria: Classification, Pathogenesis, Clinical Features, Treatment –≤ —Д–Њ—А–Љ–∞—В–µ MP3:
–Х—Б–ї–Є –Ї–љ–Њ–њ–Ї–Є —Б–Ї–∞—З–Є–≤–∞–љ–Є—П –љ–µ
–Ј–∞–≥—А—Г–Ј–Є–ї–Є—Б—М
–Э–Р–Ц–Ь–Ш–Ґ–Х –Ч–Ф–Х–°–ђ –Є–ї–Є –Њ–±–љ–Њ–≤–Є—В–µ —Б—В—А–∞–љ–Є—Ж—Г
–Х—Б–ї–Є –≤–Њ–Ј–љ–Є–Ї–∞—О—В –њ—А–Њ–±–ї–µ–Љ—Л —Б–Њ —Б–Ї–∞—З–Є–≤–∞–љ–Є–µ–Љ –≤–Є–і–µ–Њ, –њ–Њ–ґ–∞–ї—Г–є—Б—В–∞ –љ–∞–њ–Є—И–Є—В–µ –≤ –њ–Њ–і–і–µ—А–ґ–Ї—Г –њ–Њ –∞–і—А–µ—Б—Г –≤–љ–Є–Ј—Г
—Б—В—А–∞–љ–Є—Ж—Л.
–°–њ–∞—Б–Є–±–Њ –Ј–∞ –Є—Б–њ–Њ–ї—М–Ј–Њ–≤–∞–љ–Є–µ —Б–µ—А–≤–Є—Б–∞ ClipSaver.ru
Urticaria: Classification, Pathogenesis, Clinical Features, Treatment
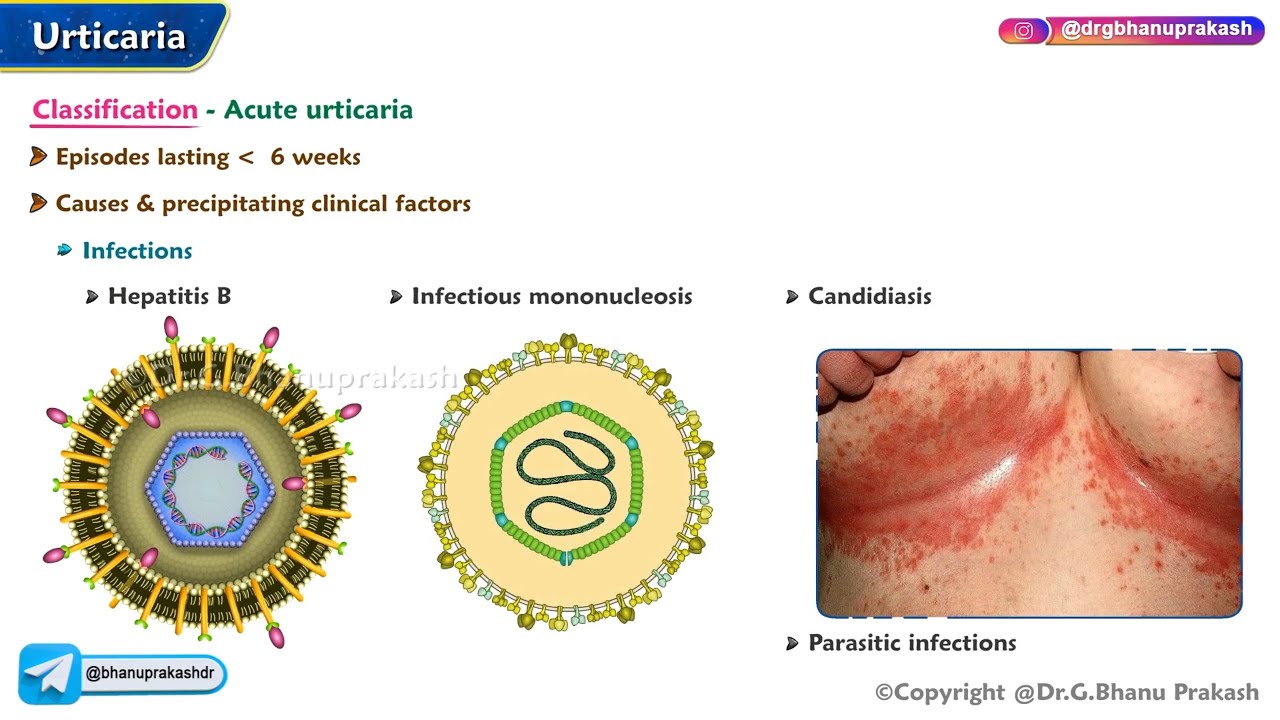
рЯУМ рЭРЕрЭР®рЭР•рЭР•рЭР®рЭР∞ рЭР®рЭРІ рЭРИрЭРІрЭРђрЭР≠рЭРЪрЭР†рЭРЂрЭРЪрЭР¶:- ¬†¬†/¬†drgbhanuprakash¬†¬† рЯУМрЭЧЭрЭЧЉрЭЧґрЭЧї рЭЧҐрЭШВрЭЧњ рЭЧІрЭЧ≤рЭЧєрЭЧ≤рЭЧірЭЧњрЭЧЃрЭЧЇ рЭЧЦрЭЧµрЭЧЃрЭЧїрЭЧїрЭЧ≤рЭЧє рЭЧЫрЭЧ≤рЭЧњрЭЧ≤:- https://t.me/bhanuprakashdr рЯУМрЭЧ¶рЭШВрЭЧѓрЭШАрЭЧ∞рЭЧњрЭЧґрЭЧѓрЭЧ≤ рЭЧІрЭЧЉ рЭЧ†рЭШЖ рЭЧ†рЭЧЃрЭЧґрЭЧєрЭЧґрЭЧїрЭЧі рЭЧЯрЭЧґрЭШАрЭШБ:- https://linktr.ee/DrGBhanuprakash Urticaria: Classification, Pathogenesis, Clinical Features, Treatment - ------------------------------------------------------------------------------------------------------------------- Introduction to Urticaria - Urticaria, commonly known as hives, is a skin condition characterized by the sudden appearance of raised, itchy welts that are often red or pale. These lesions are transient, lasting from a few hours to days, and may appear anywhere on the body. Urticaria can be either acute (lasting less than 6 weeks) or chronic (lasting more than 6 weeks). It is caused by histamine release from mast cells and basophils in the skin, leading to localized vasodilation, increased vascular permeability, and edema. Classification of Urticaria рЯУК- Urticaria is classified based on the underlying trigger and duration: Acute Urticaria: Lasts less than 6 weeks. Common causes include infections, food allergies, drug reactions, or insect bites. Chronic Urticaria: Persists for more than 6 weeks and is often idiopathic (no identifiable cause). Can be associated with autoimmune disorders or persistent infections. Physical Urticaria: Triggered by physical stimuli, such as: Dermatographism: Urticaria caused by friction or scratching. Cold urticaria: Triggered by cold exposure. Solar urticaria: Triggered by sunlight. Pressure urticaria: Caused by sustained pressure on the skin (e.g., from tight clothing). Cholinergic urticaria: Triggered by heat, exercise, or emotional stress. Contact Urticaria: Direct contact with substances like latex, plants, or chemicals causes urticaria. Hereditary Angioedema: A genetic form of urticaria that includes swelling (angioedema) in deeper layers of the skin. Pathogenesis of Urticaria рЯ¶†- The development of urticaria involves the activation of mast cells and basophils, which release histamine and other inflammatory mediators. The key steps include: Mast cell activation: Triggers can be allergens, physical stimuli, or autoimmune mechanisms. Histamine release: Leads to vasodilation and increased vascular permeability, resulting in swelling, redness (erythema), and itching. Edema: Fluid leakage from blood vessels into the surrounding tissue causes the characteristic raised wheals. Immune response: Urticaria can be mediated by IgE antibodies in allergic reactions, but in chronic cases, it may be driven by autoimmune processes where the body attacks its own IgE receptors on mast cells. Clinical Features of Urticaria рЯІР- Wheals (Hives): The primary lesion is a raised, red or skin-colored welt that is itchy and typically surrounded by erythema (redness). These wheals can vary in size, from small lesions to large plaques, and they change shape, moving from one area to another. Pruritus (Itching): Intense itching is a hallmark of urticaria, exacerbated by heat and stress. Angioedema: In some cases, deeper layers of the skin are affected, leading to angioedema, which presents as swelling, particularly in the face, lips, tongue, hands, feet, and genitals. Episodic nature: Lesions may come and go over the course of a day, resolving without leaving scars. Triggers: Episodes may be triggered by allergens (foods, medications), infections, environmental factors, or physical stimuli (e.g., pressure, heat). Treatment of Urticaria рЯТК- Management of urticaria focuses on relieving symptoms and preventing triggers: Antihistamines: First-line treatment: H1 antihistamines (e.g., cetirizine, loratadine, diphenhydramine) block histamine receptors and reduce itching and wheal formation. In chronic or severe cases, H2 antihistamines (e.g., ranitidine) may be added to enhance relief. Corticosteroids: Oral corticosteroids (e.g., prednisone) are used for short-term control of severe, acute urticaria but are not recommended for long-term use due to side effects. Omalizumab: A monoclonal antibody that blocks IgE, effective in treating chronic urticaria that is resistant to antihistamines. Epinephrine (Adrenaline): For anaphylaxis or severe angioedema with breathing difficulty, epinephrine injection is used as an emergency treatment. #Urticaria #Hives #AllergyRelief #SkinCare #Dermatology #MedicalEducation #UrticariaTreatment #ChronicUrticaria #SkinHealth #Antihistamines #MedStudentLife #ItchySkin #Immunology #medicalanimations #fmge #fmgevideos #rapidrevisionfmge #fmge2024 #mbbslectures #nationalexitexam #nationalexittest #neetpg #usmlepreparation #usmlestep1 #fmge #usmle #drgbhanuprakash #medicalstudents #medicalstudent #medicalcollege #neetpg2025 #usmleprep #usmlevideos #usmlestep1videos #medicalstudents #neetpgvideos #usmlestep2videos









