Cardiac Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations скачать в хорошем качестве
Повторяем попытку...
Скачать видео с ютуб по ссылке или смотреть без блокировок на сайте: Cardiac Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations в качестве 4k
У нас вы можете посмотреть бесплатно Cardiac Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations или скачать в максимальном доступном качестве, видео которое было загружено на ютуб. Для загрузки выберите вариант из формы ниже:
-
Информация по загрузке:
Скачать mp3 с ютуба отдельным файлом. Бесплатный рингтон Cardiac Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations в формате MP3:
Если кнопки скачивания не
загрузились
НАЖМИТЕ ЗДЕСЬ или обновите страницу
Если возникают проблемы со скачиванием видео, пожалуйста напишите в поддержку по адресу внизу
страницы.
Спасибо за использование сервиса ClipSaver.ru
Cardiac Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations
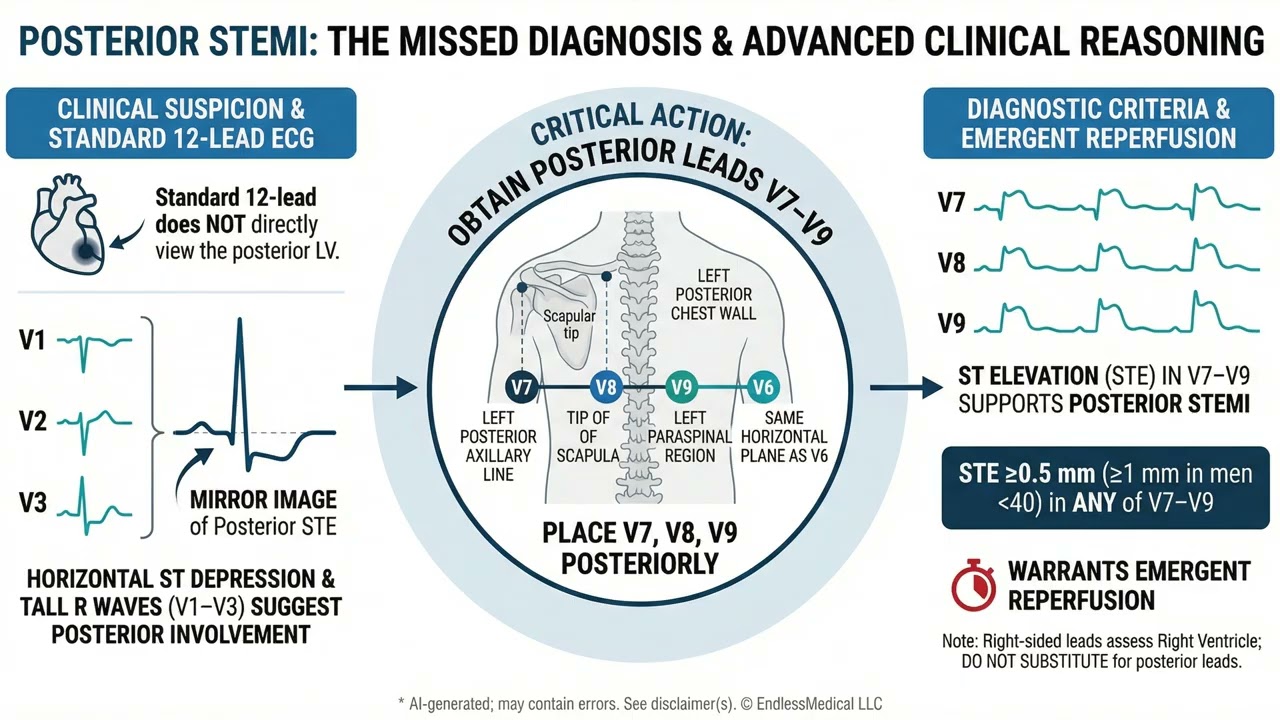
A 40-year-old man with a history of iron deficiency anemia presents with sudden crushing substernal chest pain radiating to the left shoulder and jaw, severe hypertension, diaphoresis, and worrisome ECG changes, including anterior ST depression with tall R waves. How should you approach identifying the anatomic site of myocardial ischemia using additional ECG leads? What clinical cues should guide your localization strategy in this urgent cardiac scenario? VIDEO INFO Category: Cardiac Anatomy, Human Anatomy, USMLE Step 1 Difficulty: Hard - Advanced level - Challenges experienced practitioners Question Type: Clinical Pitfalls Case Type: Emergency - Emergency scenario requiring urgent decision-making Explore more ways to learn on this and other topics by going to https://endlessmedical.academy/auth?h... QUESTION A 40-year-old man with iron deficiency anemia and a remote episode of disseminated intravascular coagulation during a complicated appendectomy at age 27 presents with crushing substernal pressure radiating to the left shoulder and jaw that started 50 minutes ago while walking to a bus stop. He quit smoking 3 years ago after 25 years of 2 packs/day (50 pack-years). He follows a vegetarian diet, denies cocaine or amphetamine use, and reports intermittent palpitations without prior syncope.... OPTIONS A. Place posterior leads V7-V9 in the same horizontal plane as V6-V7 at the left posterior axillary line, V8 at the tip of the left scapula, and V9 at the left paraspinal region-which directly view the posterior (inferobasal) left ventricular wall. B. Place right-sided precordial leads V3R-V6R across the right anterior chest to assess the posterior wall, because right-sided leads directly face the inferobasal myocardium supplied by the posterior descending artery. C. Move standard precordial leads V1-V3 cephalad to the second intercostal spaces to create high anterior leads that detect posterior wall transmural injury without placing posterior electrodes. D. Insert a single esophageal lead posterior to the left atrium to visualize the posterior left ventricular free wall more accurately than surface electrodes V7-V9 in suspected posterior STEMI. CORRECT ANSWER A. Place posterior leads V7-V9 in the same horizontal plane as V6-V7 at the left posterior axillary line, V8 at the tip of the left scapula, and V9 at the left paraspinal region-which directly view the posterior (inferobasal) left ventricular wall. EXPLANATION The ECG shows horizontal ST depression in V1-V3 with tall R waves and upright T waves, plus inferior changes-an ischemic mirror pattern suggestive of posterior transmural injury with a concomitant inferior infarction. The standard 12-lead does not directly view the posterior left ventricular wall, so supplemental posterior leads are necessary. Placing V7-V9 in the same horizontal plane as V6-V7 at the left posterior axillary line, V8 at the tip of the left scapula, V9 at the left paraspinal region-directly faces the inferobasal (posterior) LV. Per contemporary chest pain and ACS guidelines, =0.5 mm ST elevation in any of V7-V9 supports posterior STEMI and should prompt emergent reperfusion. The other options mislocalize anatomy or use nonstandard methods. Right-sided precordial leads V3R-V6R interrogate the right ventricle, not the posterior LV. Moving V1-V3 cephalad creates high anterior leads that are intended for suspected high anterior or septal ischemia, not posterior injury.... --------------------------------------------------- Our cases and questions come from the https://EndlessMedical.Academy quiz engine - multi-model platform. Each question and explanation is forged by consensus between multiple top AI models (GPT, Claude, Grok, etc.), with automated web searches for the latest research and verified references. Calculations (e.g. eGFR, dosages) are checked via code execution to eliminate errors, and all references are reviewed by several AIs to minimize hallucinations. Important note: This material is entirely AI-generated and has not been verified by human experts; despite stringent consensus checks, perfect accuracy cannot be guaranteed. Exercise caution - always corroborate the content with trusted references or qualified professionals, and never apply information from this book to patient care or clinical decisions without independent verification. Clinicians already rely on AI and online tools - myself included - so treat this book as an additional focused aid, not a replacement for proper medical education. Visit https://endlessmedical.academy for more AI-supported resources and cases. This material can not be treated as medical advice. May contain errors. ---------------------------------------------------



















