Lower Limb Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations скачать в хорошем качестве
Повторяем попытку...
Скачать видео с ютуб по ссылке или смотреть без блокировок на сайте: Lower Limb Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations в качестве 4k
У нас вы можете посмотреть бесплатно Lower Limb Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations или скачать в максимальном доступном качестве, видео которое было загружено на ютуб. Для загрузки выберите вариант из формы ниже:
-
Информация по загрузке:
Скачать mp3 с ютуба отдельным файлом. Бесплатный рингтон Lower Limb Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations в формате MP3:
Если кнопки скачивания не
загрузились
НАЖМИТЕ ЗДЕСЬ или обновите страницу
Если возникают проблемы со скачиванием видео, пожалуйста напишите в поддержку по адресу внизу
страницы.
Спасибо за использование сервиса ClipSaver.ru
Lower Limb Anatomy, Human Anatomy, USMLE Step 1 - Full Vignette with Extended Explanations
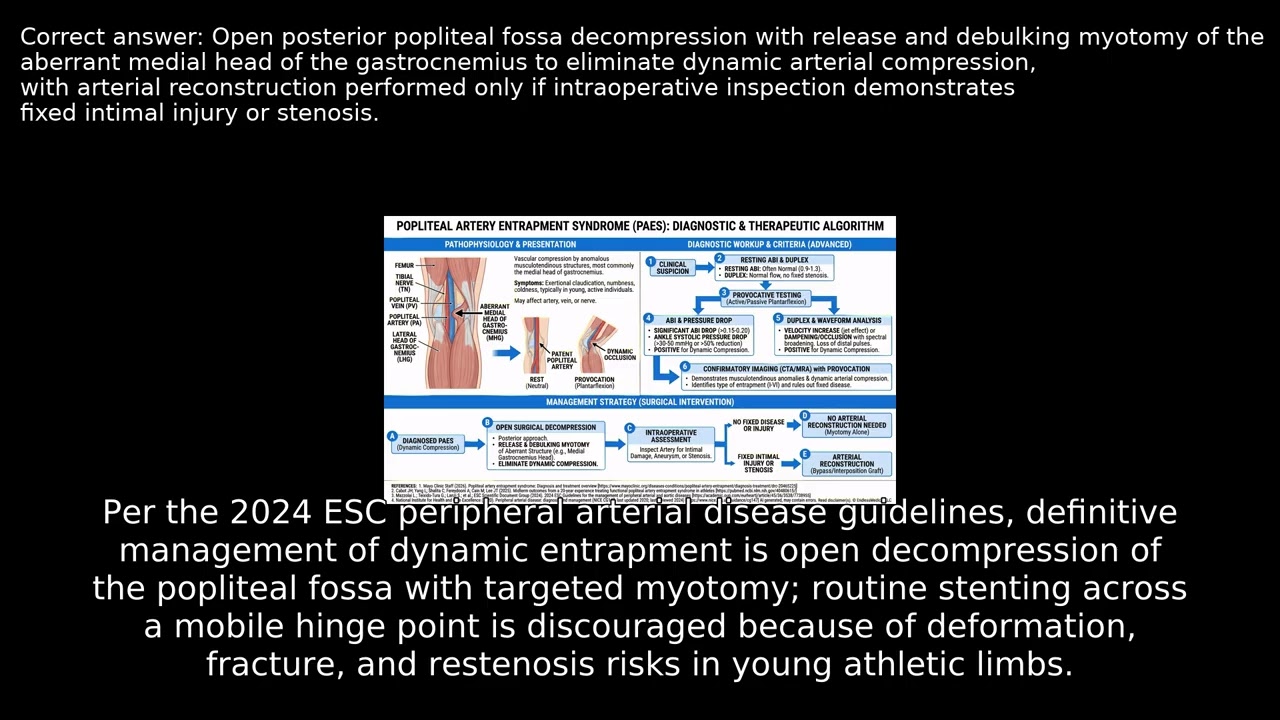
A 30-year-old recreational runner reports over a year of exertional posterior-calf tightness and plantar forefoot numbness reliably triggered by activity, resolving rapidly with rest. He notes coldness in the foot after exercise and occasional lateral-foot paresthesias with hill sprints. Despite normal pulses and strength at rest, symptoms recur with specific provocative maneuvers. What underlying mechanism best explains this patient's reproducible exertional symptoms and guides definitive management? VIDEO INFO Category: Lower Limb Anatomy, Human Anatomy, USMLE Step 1 Difficulty: Hard - Advanced level - Challenges experienced practitioners Question Type: Treatment - Evaluate therapeutic interventions and management Case Type: Rare Presentation Explore more ways to learn on this and other topics by going to https://endlessmedical.academy/auth?h... QUESTION A 30-year-old man who runs recreationally presents with 14 months of exertional posterior-calf tightness and plantar forefoot numbness that begin reliably after 600-800 meters and resolve within 2-3 minutes of rest. He notes cold feet after intervals and intermittent lateral-foot paresthesias during hill sprints. He denies rest pain, tissue loss, night pain, or color change at baseline.... OPTIONS A. Open posterior popliteal fossa decompression with release and debulking myotomy of the aberrant medial head of the gastrocnemius to eliminate dynamic arterial compression, with arterial reconstruction performed only if intraoperative inspection demonstrates fixed intimal injury or stenosis. B. Percutaneous transluminal angioplasty with primary nitinol stent placement across the dynamically compressed popliteal segment identified on provocative CT angiography, without surgical release of the compressive myofascial structures. C. Four-compartment leg fasciotomy for suspected chronic exertional compartment syndrome as the sole procedure, without targeted decompression of the popliteal artery behind the knee. D. External neurolysis of the common fibular nerve at the fibular neck to treat exercise-induced paresthesias, without addressing the popliteal fossa arterial compression. CORRECT ANSWER A. Open posterior popliteal fossa decompression with release and debulking myotomy of the aberrant medial head of the gastrocnemius to eliminate dynamic arterial compression, with arterial reconstruction performed only if intraoperative inspection demonstrates fixed intimal injury or stenosis. EXPLANATION This vignette describes functional popliteal artery entrapment syndrome with exertional, posture-dependent ischemia confirmed by dynamic duplex and provocative CTA. The best answer is surgical release of the compressive myofascial structures with selective arterial repair when, and only when, fixed intimal injury is present. Per the 2024 ESC peripheral arterial disease guidelines, definitive management of dynamic entrapment is open decompression of the popliteal fossa with targeted myotomy; routine stenting across a mobile hinge point is discouraged because of deformation, fracture, and restenosis risks in young athletic limbs. Here, resting ABI is borderline at 0.894 and falls to 0.530 with plantarflexion, a reproducible hemodynamic drop that normalizes with relaxation, and imaging shows medial deviation and dynamic compression by the medial head of gastrocnemius without fixed plaque or thrombus-findings that point to a structural compression best treated by release and not by endovascular scaffolding. The incorrect options each miss the pathophysiology.... --------------------------------------------------- Our cases and questions come from the https://EndlessMedical.Academy quiz engine - multi-model platform. Each question and explanation is forged by consensus between multiple top AI models (GPT, Claude, Grok, etc.), with automated web searches for the latest research and verified references. Calculations (e.g. eGFR, dosages) are checked via code execution to eliminate errors, and all references are reviewed by several AIs to minimize hallucinations. Important note: This material is entirely AI-generated and has not been verified by human experts; despite stringent consensus checks, perfect accuracy cannot be guaranteed. Exercise caution - always corroborate the content with trusted references or qualified professionals, and never apply information from this book to patient care or clinical decisions without independent verification. Clinicians already rely on AI and online tools - myself included - so treat this book as an additional focused aid, not a replacement for proper medical education. Visit https://endlessmedical.academy for more AI-supported resources and cases. This material can not be treated as medical advice. May contain errors. ---------------------------------------------------

![Анатомическое положение и направления [Анатомия УПРОЩЕНА]](https://image.4k-video.ru/id-video/t6-ueqFK1IE)

















